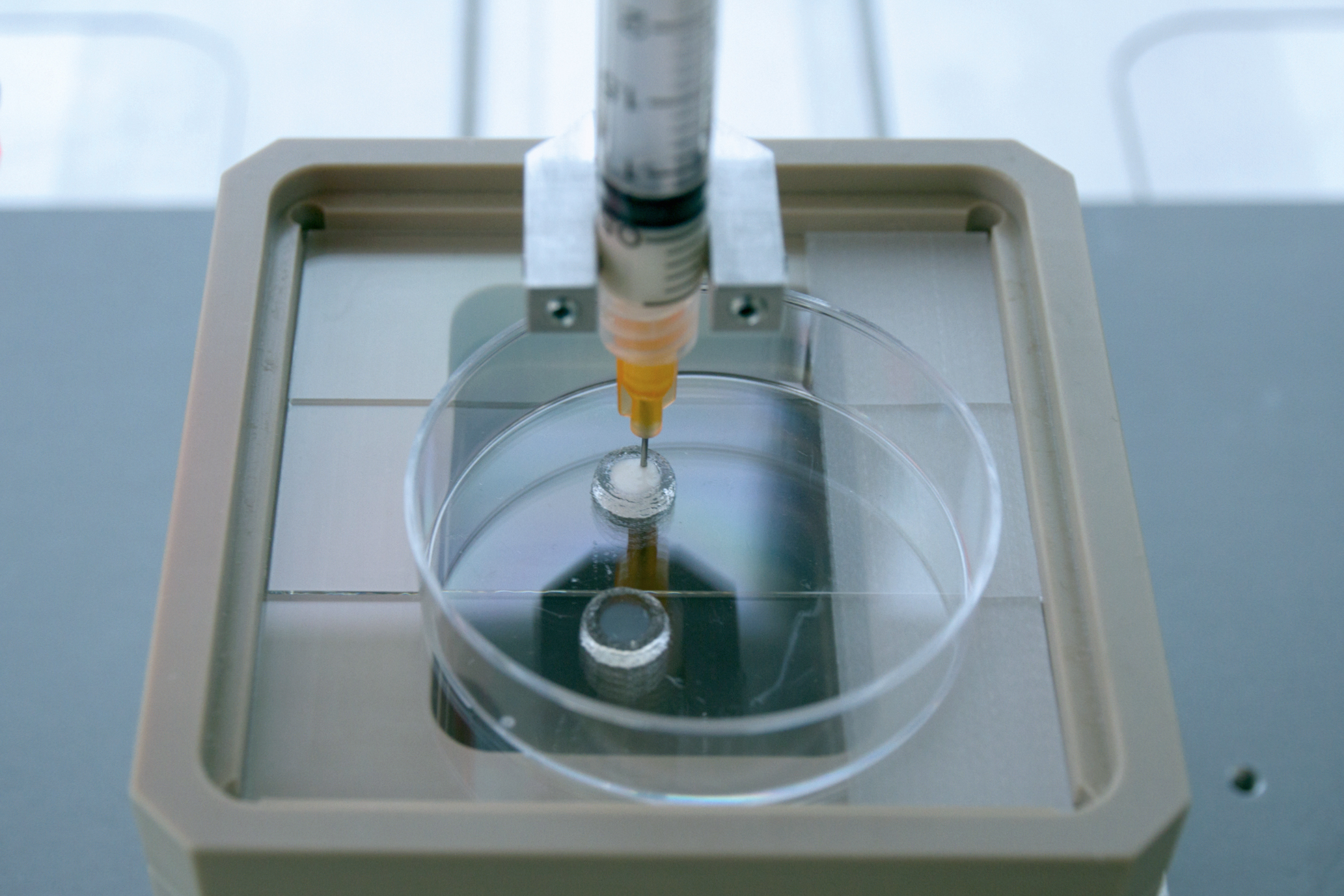
"In order to build tissues in the lab that work just as well as their natural counterparts, we need not only the best possible biomaterials, but also production processes that limit us as little as possible in terms of shaping," explains Borchers.
“Additive methods offer great flexibility in this respect. With their help, three-dimensional objects that were previously designed on the computer can now be fabricated layer by layer,” says Weber. Flexible shaping is particularly important in terms of the vision of generating personalized printed biological implants. Because modern diagnostic imaging modalities, which are currently already frequently used in daily medical practice, can provide the very digital 3D data required for customized implants.
“The additive processing of tissue matrix and cells into tissue models offers yet another advantage – automation and digital control could in the future guarantee that production can take place under controlled and standardized conditions,” adds Borchers.
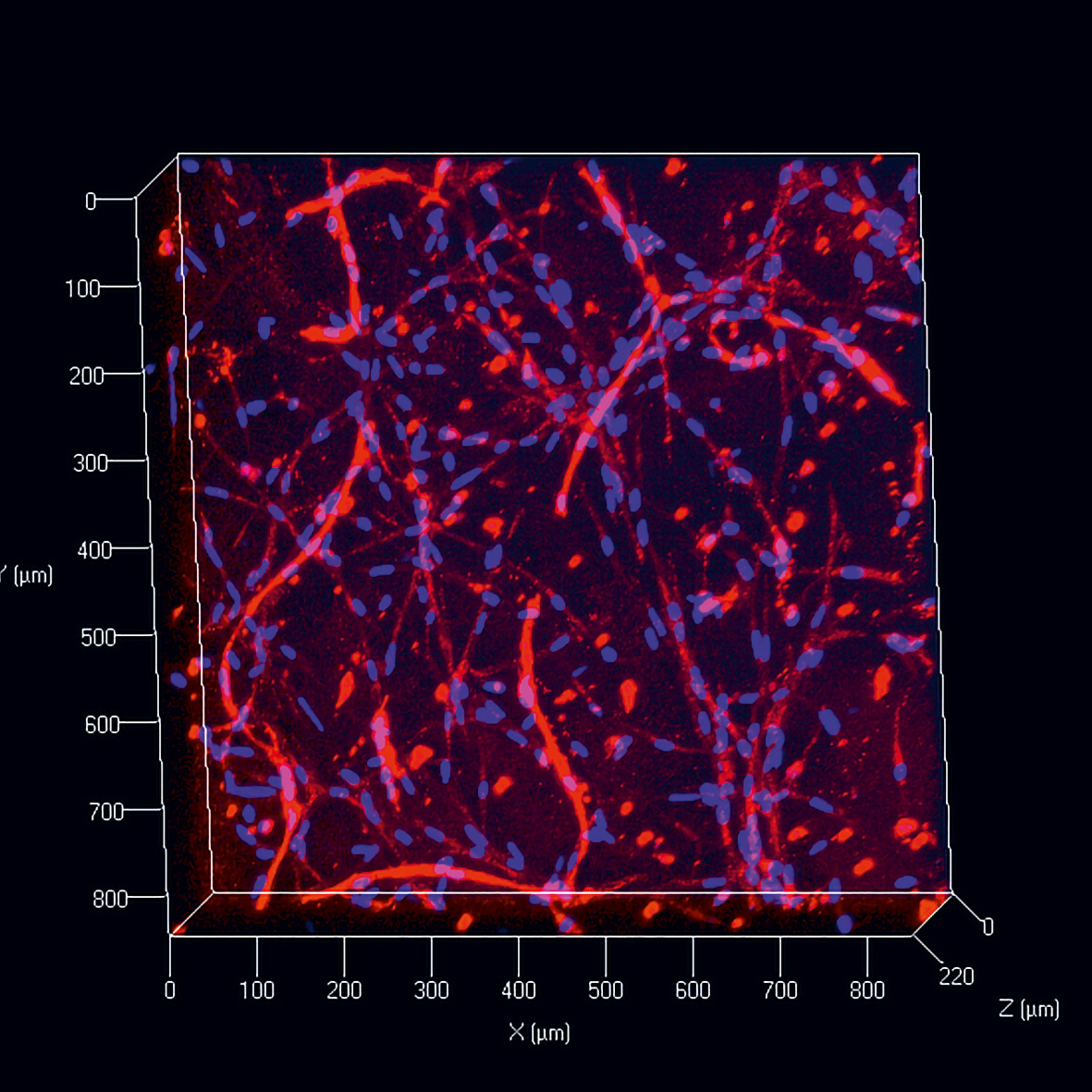
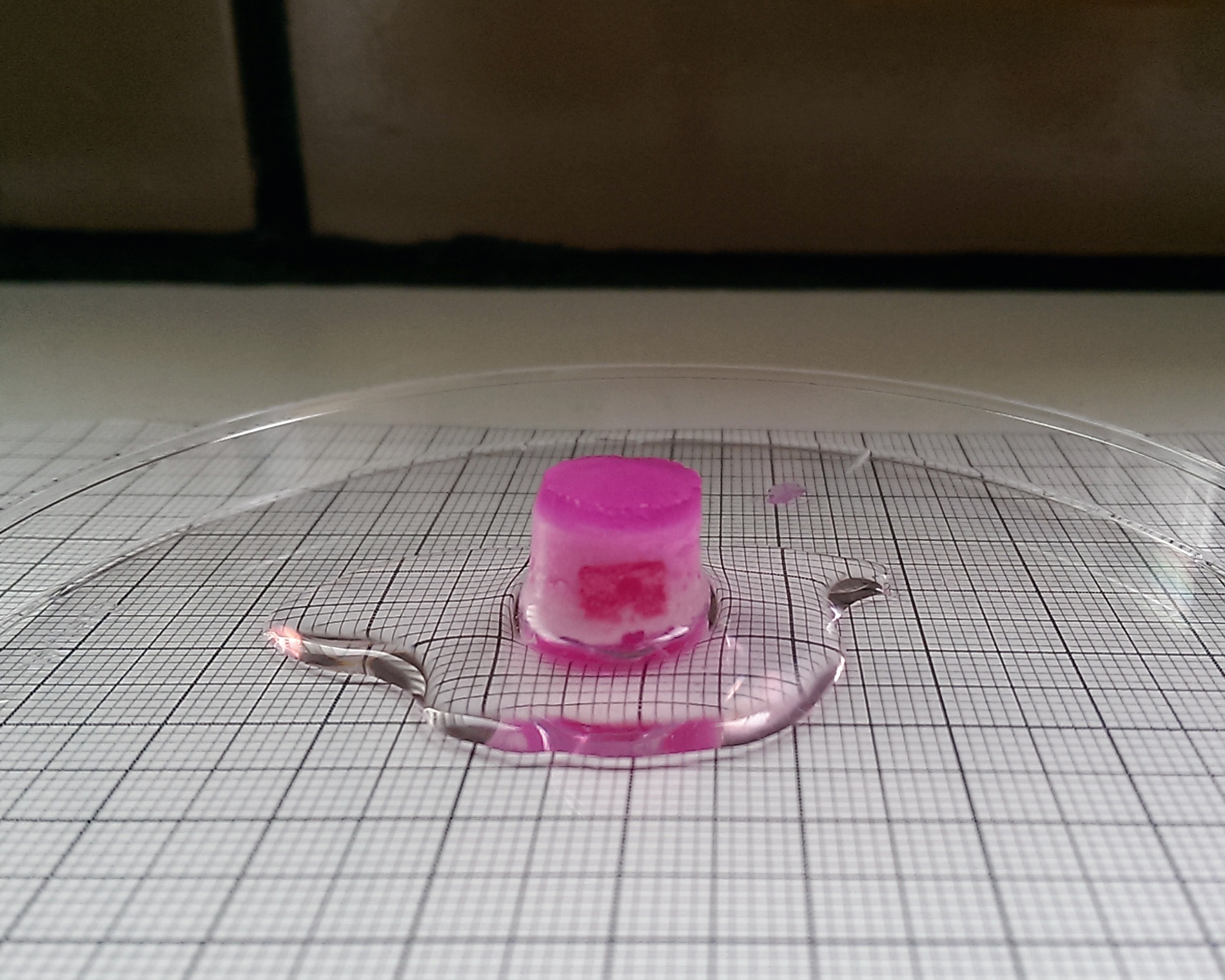
In the current state of the art, 3D printing methods are used to combine different cells and biomaterials as well as structures such as perfusion channels for suppling the cells in simply constructed tissue models [1]. The branch of research that deals with the fabrication of biological structures using additive manufacturing processes is known as bioprinting.
 Fraunhofer Institute for Interfacial Engineering and Biotechnology IGB
Fraunhofer Institute for Interfacial Engineering and Biotechnology IGB